Reflections from AHA25: What We Learned About Women’s Heart Health, Prevention, and the Power of Group-Based Care

The American Heart Association’s Scientific Sessions always feel like a glimpse into cardiology’s near-future: four days where the field’s brightest minds gather to debate, challenge, and imagine what better heart health could look like. This year in New Orleans, Systole Health had the privilege of contributing to that conversation by presenting two new studies from our women’s group-based virtual care program.
For our co-founder and COO, Lauren McConnell, and our senior primary care physician, Dr. Jen Burke-Krieg, AHA25 wasn’t just a moment to share early results. It was a chance to see where the field is heading and where women’s prevention still needs new ideas, new models, and frankly, a new imagination.

Presenting New Research: Two Posters, One Theme
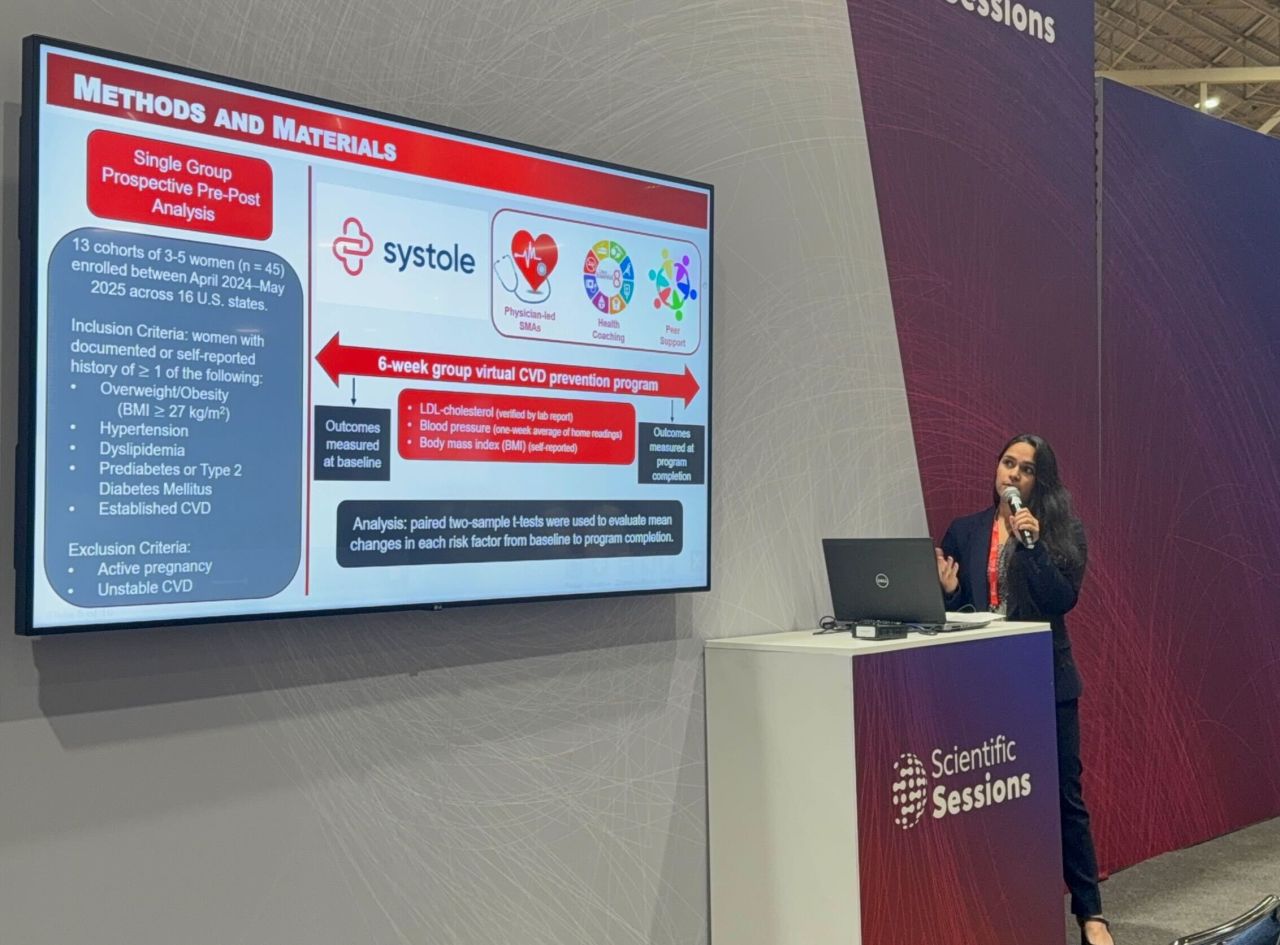
Across three days, our team presented findings from our first patient cohorts: research focused on the simple but powerful hypothesis that care delivered in community can create better outcomes than care delivered alone.
On November 8, we shared our study:
Group Virtual Care for Women with Cardiovascular-Kidney-Metabolic Syndrome.
This work explored how connection, education, and multidisciplinary guidance affect women with intersecting CKM risks, a population historically underserved in cardiology research and routine care.
On November 10, we returned with:
Closing Prevention Gaps in Women’s Heart Health: Real-World Impact of a Scalable Group Virtual Care Model.
This second poster focused on outcomes– what actually changes when women receive prevention-forward care in a small, supportive group setting.
Together, these studies underline what we believe to our core: when you bring women together, give them the right clinical tools, and surround them with evidence-based guidance, you create the conditions for better long-term heart health.
What the Data Shows So Far
The early signals are meaningful.
Our first publication highlighted strong engagement, attendance, and patient satisfaction; indicators that women aren’t just willing to participate in prevention, but eager to when the experience is designed around their realities rather than around the constraints of a traditional clinic visit.
Our second poster turned to measurable improvement:
- Reductions in LDL cholesterol
- Lower blood pressure
- Meaningful shifts in BMI
These gains emerged after just six weeks in our virtual program. Six weeks of group visits. Six weeks of combining medical guidance with health coaching, community support, and prevention rooted in practical habits.
The data is early, but it’s pointing in a clear direction: group-based virtual care can move the needle on risk factors that matter for women’s long-term cardiovascular health.
Our research team deserves immense credit for getting us here: Sehej-Leen Parmar, Dr. Emily Lau, Dr. Christopher Cannon and Systole’s CEO, Dr. Simin Gharib Lee. None of these results appear by magic. They come from rigor, repetition, and the kind of teamwork that makes science possible.

What We Heard Everywhere at AHA25
AHA was crowded– both intellectually and literally– but two themes echoed loudly this year:
Lp(a) has arrived at the center of the conversation
You couldn’t walk ten feet without hearing someone talk about lipoprotein(a) on panels, in hallway debates, or on the expo floor.
And rightly so.
Knowing your Lp(a) level early offers insight into lifelong heart risk, much like knowing your blood pressure or cholesterol. For women, whose symptoms and risk patterns are often dismissed or misinterpreted, this marker becomes even more vital.
We’ve already incorporated Lp(a) testing into Systole’s baseline recommendations, anticipating the therapies now in development. Understanding your risk is the first step toward changing it.
Prevention requires better coordination… and better design
The other recurring theme was something quieter but just as urgent: patients are being asked to carry an impossible amount of responsibility.
Frequent labs.
Multiple medications.
Daily blood pressure readings.
Movement goals.
Nourishment goals.
Sleep goals.
And that’s on top of caregiving, jobs, families, commutes, and the thousand invisible tasks required to simply function in modern life.
If prevention is going to work– truly work, at scale, for real people living real lives– our systems and tools need to lighten the load, not add to it.
For us, that’s the animating question we’re bringing home from New Orleans:
How do we make the healthy thing the easiest thing for our patients?
Group-based virtual care is one answer. Human-centered design is another. Technology that supports, rather than overwhelms, is a third. What matters is that the field keeps pushing toward models where prevention is not a burden but a relief.

AHA25 Was a Beginning, Not a Finale
We left New Orleans energized by the science, by the conversations, and by the clinicians who stopped by our posters because they believe what we believe:
Women deserve better cardiovascular care.
Prevention is not optional.
Connection is a treatment modality.
Our early data reinforces that when care is delivered in community with structure, accountability, and humanity, women don’t just participate. They improve.
We’re excited to share more as our research grows, our cohorts expand, and our model continues to evolve. AHA was a milestone, but it’s also a marker of what’s ahead.
The work continues, and the future looks bright!


